Colon Cancer Stages: What Do They Mean?
Staging cancers helps doctors understand how advanced a cancer is, come up with the best treatment plan, and predict the path of the disease, including the chance of recovery.
Colon cancer is no different. There are several ways to test for what stage the colon cancer is in and monitor it while you are in treatment.
Tests for Staging Colon and Rectal Cancer
A colon cancer diagnosis or a rectal cancer diagnosis typically involves a biopsy — studying suspicious tissue from the colon or rectum under a microscope. If doctors discover cancer they will run tests to see how advanced the disease is and whether it has spread to other areas of the body.
- Biopsy A doctor may request a biopsy when an initial screening shows signs of cancer. During a biopsy, a small piece of tissue is removed from the colon and sent to a lab for evaluation. In some cases, part of the colon may need to be removed as opposed to a small sample. Depending on what the biopsy shows, a molecular test may be next to look for changes and mutations in specific genes and proteins.
- Complete Blood Count (CBC) A CBC test is typically used to determine if you are anemic, or lack red blood cells. Anemia is caused by chronic bleeding from the tumor. Iron deficiency anemia is one of the most common symptoms in colorectal cancer.
- Carcinoembryonic Antigen (CEA) A CEA test measures the amount of carcinoembryonic antigens in the blood. CEAs don’t necessarily mean you have cancer, but some types of cancer, including colorectal cancer, produce more CEA than would normally be in your body.
- Chest X-Ray Doctors may use this test to see if cancer cells have spread to the lungs, but a CT scan is more common.
- Computerized Tomography (CT or CAT) Scan In this test, cross-sectional images of the body created with X-rays are examined for signs that colorectal cancer has spread to other organs like the liver.
- Liver Enzymes Liver enzymes are used to check how well your liver is functioning. These tests can potentially show if colorectal cancer has spread to the liver.
- Magnetic Resonance Imaging (MRI) Scan Radio waves and strong magnets produce detailed images that can help doctors see cancerous growths. An endorectal MRI scans the pelvis area specifically and is used to see if the cancer has spread from the rectum to other places in the body.
- Positron Emission Tomography (PET) Scan Doctors inject a small amount of a radioactive sugar substance into the blood, then look to see how much it is absorbed by cells in different areas of the body. Cancer cells tend to absorb more of these sugars than normal cells because they require more energy to fuel their rapid growth.
- Surgery At very early stages, surgery may be used to remove all or part of a tumor, either by removing a polyp in a colonoscopy or removing a larger piece through local excision, cutting out a small cancer and some of the healthy tissue around it. These surgeries can also be used to see if the cancer cannot fully be removed by small surgeries or if it has spread through the colon.
- Ultrasound This device can spot tumors by creating sound waves and transforming echoes into images on a screen. A technician may use an abdominal ultrasound to see if there are tumors on the organs in your abdomen, such as on your liver or gallbladder. An endorectal ultrasound is used to see whether a cancer has grown through the rectal wall and spread to nearby organs. Intraoperative ultrasound is usually used during primary surgeries, or initial removals of tumors, for colorectal cancer. If a tumor is detected on the liver during the surgery, a biopsy sample is taken.
Staging Colon Cancer and Rectal Cancer
The TNM system is organized around the answers to a series of questions.
- Tumor (T) Has the tumor grown beyond the inside lining of the colon or rectum and into the wall? If so, how many layers deep is it?
- Node (N) Has the tumor spread to the lymph nodes? If so, where and how many?
- Metastasis (M) Has the cancer spread beyond the lymph nodes to other parts of the body? If so, where and how much?
Once doctors make all these assessments, they combine this information to stage the cancer.
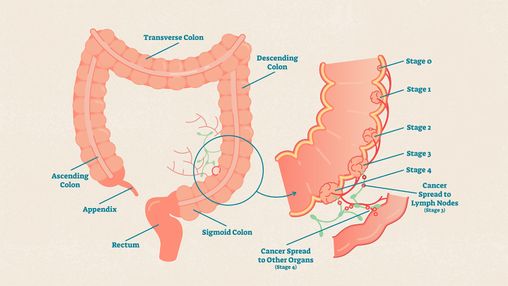
Colon and Rectal Cancer Stages
Generally, the higher the number and letter, the more advanced the cancer.
Stage 0
The cancer is in its earliest stage, called carcinoma in situ or intramucosal carcinoma. It has not grown beyond the inner layer (mucosa) of the colon or rectum (Tis, N0, M0).
Stage 1
The cancer has grown into the submucosa, and possibly into the thick muscle layer beneath it (muscularis propria). It has not spread to nearby lymph nodes or distant sites (T1 or T2, N0, M0).
Stage 2A
The cancer has grown into the colon wall or rectum but not through it. It has not reached nearby organs or lymph nodes or spread to distant sites (T3, N0, M0).
Stage 2B
The cancer has grown through the wall of the colon or rectum but not into nearby tissue or organs. It has not spread to nearby lymph nodes or distant sites (T4a, N0, M0).
Stage 2C
The cancer has grown through the wall of the colon or rectum and is attached to or has grown into other nearby tissues or organs. It has not spread to nearby lymph nodes or distant sites (T4b, N0, M0).
Stage 3A
The cancer has grown into the submucosa and possibly the muscularis propria; it has spread to 1 to 3 nearby lymph nodes or into areas of fat near the lymph nodes, but not to distant sites (T1 or T2, N1/N1c, M0).
— or —
The cancer has grown into the submucosa and spread to 4 to 6 nearby lymph nodes but not to distant sites (T1, N2a, M0).
Stage 3B
The cancer has grown into the wall of the colon or rectum or through the visceral peritoneum (the inner lining of the abdominal cavity) but has not reached nearby organs. It has spread to 1 to 3 nearby lymph nodes or into areas of fat near the lymph nodes but not to distant sites (T3 or T4a, N1/N1c, M0).
— or —
The cancer has grown into the muscularis propria or into the wall of the colon or rectum and has spread to 4 to 6 nearby lymph nodes but not to distant sites (T2 or T3, N2a, M0).
— or —
The cancer has grown into the submucosa and possibly the muscularis propria. It has spread to 7 or more nearby lymph nodes but not to distant sites (T1 or T2, N2b, M0).
Stage 3C
The cancer has grown through the wall of the colon or rectum, including the tissues lining it (the visceral peritoneum), but has not reached nearby organs. It has spread to 4 to 6 nearby lymph nodes but not to distant sites (T4a, N2a, M0).
— or —
The cancer has grown into the wall of the colon or rectum, including the visceral peritoneum, but has not reached nearby organs. It has spread to 7 or more nearby lymph nodes but not to distant sites (T3 or T4a, N2b, M0).
— or —
The cancer has grown through the wall of the colon or rectum and is attached to or has grown into nearby tissues or organs. It has spread to at least one nearby lymph node or areas of fat close to it but not to distant sites (T4b, N1 or N2, M0).
Stage 4A
The cancer has spread to one distant organ, such as the liver or lungs, or distant set of lymph nodes, but not to distant parts of the lining of the abdominal cavity, the peritoneum (any T, any N, M1a).
Stage 4B
The cancer has spread to more than one distant organ or distant set of lymph nodes, but not to distant parts of the peritoneum (any T, any N, M1b).
Stage 4C
The cancer has spread to distant parts of the peritoneum (any T, any N, M1c).
Colon and Rectal Cancer Survival Rates
For colorectal cancers, available statistics are not based on the TNM cancer staging system. They are collected by the National Cancer Institute and put into the Surveillance, Epidemiology, and End Results (SEER) database. The SEER database separates colorectal cancer into three broader groups:
- Localized If the cancer has not spread outside of the colon or rectum, it is considered localized.
- Regional The cancer is outside the colon or rectum, but only to neighboring organs or lymph nodes.
- Distant The cancer is found in farther parts of the body, such as the liver or lungs.
Here’s how the TNM stages fit into the SEER groups:
Localized
Stage 0, Stage 1, Stage 2A, Stage 2B, Stage 2C
Regional
Stage 3A, Stage 3B, Stage 3C
Distant
Stage 4A, Stage 4B, Stage 4C
Generally speaking, the more distant the cancer is from the colon or rectum, the poorer the prognosis.
However, there are many reasons to be hopeful. Over the last few decades, the death rate from colorectal cancer for older adults has been dropping, likely due to preventative screenings and polypectomies. A better understanding of the role the liver plays and checking for and removing liver tumors also greatly improved survival outcomes. And, treatments and treatment options continue to improve.
For colon cancer:
- Localized: 91 percent
- Regional: 73 percent
- Distant: 13 percent
- Group average: 63 percent
For rectal cancer:
- Localized: 90 percent
- Regional: 74 percent
- Distant: 18 percent
- Group average: 67 percent
The Takeaway
- Colorectal cancer staging is crucial in understanding colon cancer progression, guiding treatment decisions, and assessing potential outcomes.
- Major tests used to stage colon cancer include CT scans, MRIs, ultrasounds, and PET scans to determine the spread of cancer to other body parts.
- Colorectal cancer at higher stages typically indicates a poorer prognosis, but every case is unique, so it's important to have ongoing conversations with your healthcare team for personalized care.
- Treatments for colorectal cancer have greatly improved over the past few decades, and so have survival rates with better understanding of the disease.
Resources We Trust
- Mayo Clinic: Colon Cancer Screening: Weighing the Options
- Cleveland Clinic: Diet Revealed as a Main Risk Factor for Colon Cancer in Younger Adults
- National Cancer Institute: Advances in Colorectal Cancer Research
- American Cancer Society: Colorectal Cancer Quiz
- Colorectal Cancer Alliance: Colorectal Cancer Resources and Support
- Tests to Diagnose and Stage Colorectal Cancer. American Cancer Society. January 29, 2024.
- How Is a Biopsy Done? American Cancer Society. January 29, 2024.
- Chardalias L et al. Iron Deficiency Anemia in Colorectal Cancer Patients: Is Preoperative Intravenous Iron Infusion Indicated? A Narrative Review of the Literature. Cancer Diagnosis & Prognosis. March 3, 2023.
- CEA Test (Carcinoembryonic Antigen). Cleveland Clinic. April 11, 2022.
- Wang Z et al. Extracellular vesicles in fatty liver promote a metastatic tumor microenvironment. Cell Metabolism. July 11, 2023.
- Surgery for Colon Cancer. American Cancer Society. January 29, 2024.
- Colon Cancer Treatment (PDQ®)–Patient Version. National Cancer Institute. September 13, 2024.
- Coco D et al. Routine Intraoperative Ultrasound for the Detection of Liver Metastases during Resection of Primary Colorectal Cancer – A Systematic Review. Mædica. June 2020.
- Colorectal Cancer Stages. American Cancer Society. January 29, 2024.
- Survival Rates for Colorectal Cancer. American Cancer Society. January 16, 2025.
- Key Statistics for Colorectal Cancer. American Cancer Society. January 29, 2024.
- Zeineddine FA et al. Survival improvement for patients with metastatic colorectal cancer over twenty years. NPJ Precision Oncology. February 13, 2023.
- Advances in Colorectal Cancer Research. National Cancer Institute. March 4, 2024.

Conor Steuer, MD
Medical Reviewer
Conor E. Steuer, MD, is medical oncologist specializing in the care of aerodigestive cancers, mesothelioma, and thymic malignancies and an assistant professor in the department of hematology and medical oncology at the Emory University School of Medicine in Atlanta. He joined the clinical staff at Emory's Winship Cancer Institute as a practicing physician in July 2015. He currently serves as chair of the Lung and Aerodigestive Malignancies Working Group and is a member of the Discovery and Developmental Therapeutics Research Program at Winship.
Dr. Steuer received his medical degree from the New York University School of Medicine in 2009. He completed his postdoctoral training as a fellow in the department of hematology and medical oncology at the Emory University School of Medicine, where he was chief fellow in his final year.
He has been active in research including in clinical trial development, database analyses, and investigation of molecular biomarkers. He is interested in investigating the molecular biology and genomics of thoracic and head and neck tumors in order to be able to further the care of these patient populations. Additionally, he has taken an interest in utilizing national databases to perform clinical outcomes research, as well as further investigate rare forms of thoracic cancers.
Steuer's work has been published in many leading journals, such as Cancer, the Journal of Thoracic Oncology, and Lung Cancer, and has been presented at multiple international conferences.

Pamela Kaufman
Author
Pamela Kaufman assigns and edits stories about infectious diseases and general health topics and strategizes on news coverage. She began her journalism career as a junior editor on the health and fitness beat at Vogue, followed by a long stint at Food & Wine, where she rose through the ranks to become executive editor. Kaufman has written for Rutgers University and Fordham Law School and was selected for a 2022 Health Journalism Fellowship from the Association of Health Care Journalists and the Centers for Disease Control and Prevention (CDC).
Kaufman enjoys going on restaurant adventures, reading novels, making soup in her slow cooker, and hanging out with her dog. She lives in New York City with her husband and two kids.